We’re all about equipping you with the know-how to understand your symptoms, and we especially emphasize the specific, tangible ways to manage them. Our goal is to empower YOU to take charge of your menopause journey, starting today.
A quick note about product recommendations…Elektra Health is not paid to feature any products. We just like them and think you might too, though we can’t guarantee any results.
Lifestyle & Holistic Practices
Of all the integrative practices out there, we recommend vaginal dilators or internal vibrators (such as Maude or Intimate Rose) which, like intercourse, help maintain the quality of the tissue during menopause, as well as the muscles surrounding the opening of the vagina. They can also be helpful when applying moisturizers…and while we’re on the subject:
Moisturize, moisturize, moisturize your vaginal walls and your vulva!
At least three times per week, if you can. (Who said your nightly moisturizing routine was just for your face?) Unlike lubrication, which is meant for sex, vaginal moisturizers and lotions draw moisture into the vaginal and/or vulvar tissues, which typically have less elasticity during menopause due to low estrogen. We have a lot of options for moisturizers, including gels, suppositories, and natural oils.
Revaree is a hormone-free, applicator-free vaginal insert with hyaluronic acid (HA) that renews your body’s moisture. When used every 2-3 days at night, 84% of women experienced improvements in vaginal dryness, 86% experienced a reduction in vaginal itching and burning, and 57% a reduction in painful sex.
Other brands like Replens and HYALO GYN are hormone-free gels that are inserted into the vagina using applicators (somewhat similar to those you may have used for yeast infections).
Interested in the natural route? Organic coconut oil, olive oil, and vitamin E oil are also excellent options, and can be used for internal or external application. If using coconut oil, make sure it’s unrefined because it goes through less processing.
Exercise
Before going any further, we just want to say that we are NOT into the jade egg hype which, if you haven’t heard about, is essentially a rock that some (not doctors) suggested at one point could improve your sex life and balance your menstrual cycle if you put it in your vagina. Needless to say, it was immediately debunked by experts.
However, there ARE certain exercises that we do recommend to build strength along the pelvic floor and help ease menopause-related vaginal and urinary symptoms.
- Pelvic floor physical therapy: this physical therapy subspecialty focuses on the health of the pelvic floor to help with a wide variety of genitourinary issues
- Yoga poses specifically tailored to the pelvic floor: savasana with bent legs, knees to chest, warrior 2, cat-cow, wide-legged squad, and wide-legged forward fold
- Kegel exercises: imagine you are sitting on a marble, then tighten your pelvic muscles for ~3 seconds as if you’re lifting up the marble. Relax for a count of three and repeat. Be sure not to contract your abdominal muscles as you do so – put your hand on your belly to make sure you don’t feel your muscles tighten. Kegels help with stress and urge incontinence (when you leak urine when sneezing or jumping, or when you’re about to go to the bathroom). Kegels aren’t for everyone, though. If you experience pain or difficulty with vaginal penetration, that may be a sign of a tight pelvic floor, which kegel exercises can actually worsen. Not sure what’s going on down there? Definitely reach out to a pelvic floor therapist — or Elektra Health!
Supplements & Over-the-Counter Solutions
Supplements and over-the-counter solutions can be effective in managing vaginal and vulvar symptoms…if you choose wisely. We recommend consulting with your healthcare provider first to ensure you’re using something with optimal efficacy and safety (i.e. backed by clinical research) or consulting with Elektra’s providers. Here’s a quick primer from our team on how to go about selecting high-quality supplements.
Membrasin is an estrogen-free nutritional supplement that supports healthy vaginal function and helps you produce your own moisture, naturally. The active ingredient, SBA24 (sea buckthorn oil) has been found to improve the integrity of the vaginal lining by 50%, with users experiencing double the improvement in dryness compared to the placebo group. Most of us have probably NOT heard of sea buckthorn oil (just an inkling, really), but we love to see that it’s backed by research on efficacy.
Wearables
For some women, pain during sex can be caused by penetration that is too deep. The Ohnut is a wearable designed to be worn at the base of the penis, and can be adjusted to limit depth of penetration.
Prescriptions
Hormonal
Because vaginal symptoms are primarily a result of decreased estrogen, certain women turn to hormone replacement therapy (HRT) as an effective treatment. It essentially involves taking a supplemental form of either estrogen or estrogen and progesterone to balance out the two and replace what the body is no longer producing.
There are over 10 types of hormone therapy, which can be broken down into categories based on origin, composition, type of manufacturing, and whether they affect the whole body or are active locally. Here’s what you need to know about local vs systemic HRT for vaginal symptoms:
Local HRT
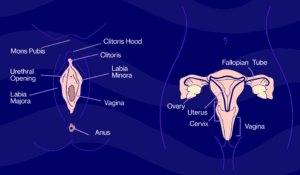
As its name suggests, local HRT acts on a specific part of the body and is a great option for managing vaginal symptoms — hormones can be applied directly to the vagina and occasionally, the vulva. This is typically done with low-dose estrogen and occasionally with DHEA (a hormone produced naturally in your adrenal glands that’s converted by the body into estrogen).
Local vaginal estrogen replacement is often the first line treatment for genitourinary symptoms of menopause, and has been shown time and time again to be beneficial for vaginal dryness, pain during intercourse after menopause, and even bladder health (by decreasing frequent UTIs for example). Some of us need hormones applied to the vulva or vestibule (entrance to the vagina) in addition to vaginal application.
And unlike systemic HRT, these local options don’t carry the same risks since they’re designed to only be active vaginally. Studies show that low dose vaginal estrogen therapies have very low systemic absorption, making them safe for individuals with a history of blood clots, coronary artery disease, or stroke, and research confirms no increased risk of cardiovascular disease or cancer from their use. And while this means they won’t do much for hot flashes, they are considered to be safe for most women, even those with a history of breast cancer. If this is you, then it’s worth talking to your oncologist about vaginal estrogen for your symptoms.
Local HRT is a great option for managing vaginal symptoms – and it’s safe for most women!
There are a number of options, including tablets (Vagifem, Vuvafem), inserts (Imvexxy), creams (Estrace, Premarin), rings (Estring) or suppositories (Intrarosa). We encourage you to discuss these and make the best choice for you with your provider or with us.
Systemic HRT
Systemic, on the other hand, is absorbed throughout the body to target menopause symptoms such as hot flashes, night sweats, and PMS. Examples here include gels, patches, pills, and creams.
Ospemifene (brand name: Osphena) is an FDA-approved, selective estrogen receptor modulator (SERM). While not a hormone per se, it does affect the way estrogen works in the body. It comes in the form of a pill taken daily; however, hot flashes can be a side effect — in trials, 4-8% more women experience hot flashes compared to placebo. This drug is not advised for women with a high risk or history of breast cancer.
For a full run-down on HRT refer to our complete guide.
Laser & Radiofrequency Treatments
Recently, certain in-office procedures advertised for menopausal vaginal changes are gaining in popularity, including laser devices such as Mona Lisa and Femtouch, and radiofrequency devices such as Thermiva or Viveve.
Unfortunately, research is mixed on these and they are not FDA approved for treatment of menopausal vaginal complaints as of now. Additionally, they are typically considered elective procedures and therefore result in higher out of pocket costs. However, for women who are not willing or are unable to use other therapies, they may represent an option, as long as proper counseling is done about their risks, benefits, cost, and need for additional procedures.
Dig Deeper
Sex Without Pain: A Self-Treatment Guide To The Sex Life You Deserve by Heather Jeffcoat, DPT
We’re always keeping an eye out on emerging research and the latest clinical studies. Subscribe to our weekly Elektra Digest for the latest, science-based info direct to your inbox. Something work well for you that’s not listed here? We want to hear it! Shoot us a note at [email protected]. (We’re human, promise.)
Pro tip #2
If your vulvar tissues are tender, be sure to moisturize as often as needed. Use your fingers to apply moisturizers directly to your skin. You can apply whenever and as often as needed, but before bed is ideal as it can be fully absorbed. If wiping hurts, pat dry and upgrade to softer toilet paper if needed (stay away from scented, dyed, or aloe brands). To prevent irritation, wear 100% cotton underwear, use “free and clear” detergents, and skip fabric softener and dryer sheets. Basic soap and water is best for cleaning the vulva — nothing with scents. And...NEVER EVER douche.
Pro tip #3
Here are strategies that can help you get more comfortable (and confident!) seeking medical advice from your doctor about vulvovaginal symptoms:
1. Write down your questions so you won’t forget them when in the exam room.
2. Give your provider a head’s up pre-visit via the nurse or assistant who does your vitals.
3. Realize that you’re not alone! Your provider has definitely heard about these same issues before.
Disclaimer: This information is for general educational purposes, and should not be used as a substitute for medical advice, diagnosis, or treatment of any health condition or problem.
As with anything you put into your body, taking dietary supplements can also involve health risks. You should consult a medical professional before taking supplements and inform your doctor about any supplements, as well as any medications you already take, since there may be interactions.
Helpful? Share the wealth!
Share with a friend who deserves evidence-based expertise &
solutions.